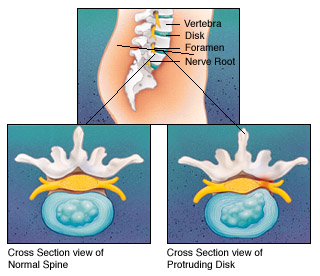
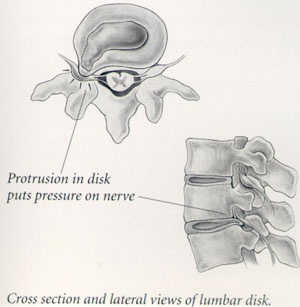
Herniated Nucleus Pulposus- HERNIATED DISC - DefinitionA herniated disc is a fragment of the disc nucleus which is pushed out of the outer disc margin, into the spinal canal through a tear or "rupture." In the herniated disc's new position, it presses on spinal nerves, producing pain down the accompanying leg. This produces a sharp, severe pain down the entire leg and into the foot. The spinal canal has limited space which is inadequate for the spinal nerve and the displaced herniated disc fragment.The compression and subsequent inflammation is directly responsible for the pain one feels down the leg, termed "sciatica." The direct compression of the nerve may produce weakness in the leg or foot in a specific patter, depending upon which spinal nerve is compressed.
A herniated disc is a definite displaced fragment of nucleus pushed
out through a tear in the outer layer of the disc (annulus). For a disc
to become herniated, it typically is in an early stage of degeneration.
Typical Pain and FindingsTypically, a herniated disc is preceded by an episode of low back pain or a long history of intermittent episodes of low back pain. However, when the nucleus actually herniates out through the annulus and compresses the spinal nerve, then the pain typically changes from back pain to sciatica. Sciatica is sharp pain which radiates from the low back area down through the leg, into the foot in a characteristic pattern, depending upon the spinal nerve affected. This pain often is described as sharp, electric shock-like, sever with standing, walking or sitting. The pain is frequently relieved by lying down or utilizing a lumbar support chair or insert.There also may be resulting leg muscle weakness from a compromise of the spinal nerve affected. Most commonly, the back pain has resolved by the time sciatica develops, or there is minimal back pain compared to the severe leg pain. The location of the leg pain is usually so specific that the doctor can indentify the disc level which is herniated. In addition to leg muscle weakness, there may also be knee or ankle reflex loss. What Diagnostic Tests are Used for EvaluationsX-rays of the low back area are obtained to search for unusual causes of
leg pain, i.e. tumors, infections, fractures, etc. An MRI of the lumbar
spine area is obtained, as this will demonstrate the degree of disc
degeneration at the herniated level, in addition to the condition of
other lumbar discs in the low back. TreatmentThe initial treatment for a herniated disc is usually conservative, i.e.
nonoperative. One usually begins with resting the low back area,
maintaining a comfortable posture and painless activity level for a few
days to several weeks. This in in order to allow the spinal nerve
inflammation to quiet down and resolve. PrognosisA person who has sustained one disc herniation is statistically at increased risk for experiencing another. There is an approximate 5% rate of recurrent disc herniation at the same level, and a lesser incidence of new disc herniation at another level. Factors involved may be weight related level of physical conditioning, work or behavioral habits. Since these factors are typically the same after surgery, there is an increased risk of herniated disc in this group, over the general population.However, the good news is that the majority of disc herniations (90%) do not require surgery, and will resolve with conservative, nonoperative treatment, without significant long-term sequelae. Unfortunately, approximately 5% of patients with herniated, degenerated discs will go on to experience symptomatic or severe and incapacitating low back pain which significantly affects their life activities and work. This unfortunate result is not always specifically the result of surgery. The causes of this unremitting pain are not always clear or agreed on, and my be from several sources. When this occurs, the prognosis is poor for returning to normal life activities regardless of age. After a successful laminotomy and discectomy, 80-85% of patients do extremely well and are able to return to their normal job in approximately six weeks time. There may be small permanent patches of numbness in the involved leg which, fortunately, are not disabling. Flare-ups or exacerbations of less severe and less significant sciatic type pain may develop in the future (usually on an infrequent basis). RecommendationsOur advice to those who have herniated disc disease is to become knowledgeable in back school lifting techniques and activity modifications from your physical therapist. Making your back strong through exercises performed for approximately 30 minutes daily will restore normal flexibility in the lumbar spine region, as well as strengthen muscles which can resist strain and repeat injury. Always avoid heavy lifting, especially in association with twisting of the lumbar spine. Protect your back for at least nine months to a year after sustaining the herniated disc.Feel free to consult your physical therapist for more specific recommendations regarding postoperative or post-herniated disc lumbar spine reconditioning and maintaining a well-conditioned spine. |